
A special contribution from Pain Concern, offering guidance and support for managing emotions alongside pain
Here we help you think about how chronic pain can give rise to difficult feelings and thoughts. We’ll look at how this can affect your life and how to address these emotional effects of pain.
Chronic pain can have a big impact on day-to-day life – relationships, daily activities, sleep, employment and all aspects of general health can be affected. These changes cause emotional strain on top of the pain. Many people experience a ‘vicious cycle’ that can make pain harder to deal with.
To think about how pain gets mixed up with emotions and the other things going on in our lives, healthcare professionals use what’s called a ‘bio-psycho-social’ model, as shown below:
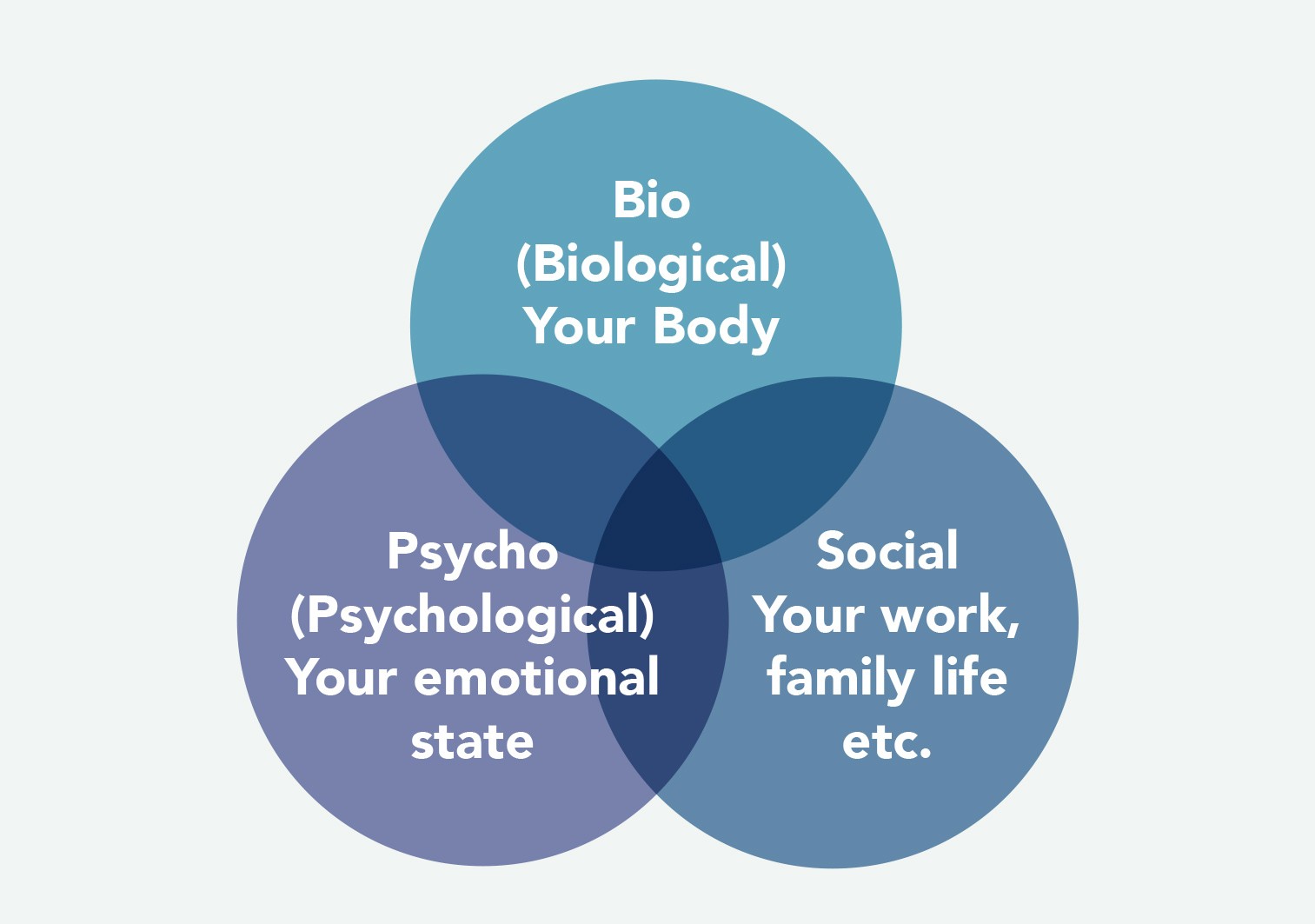
The bio-psycho-social model recognises that all three areas interact in our overall experience of pain.
Here we’ll focus on the emotional part of the pain experience. Without always having a clear picture of the cause of the pain or a recognisable diagnosis it can be difficult to consider the emotional side of pain without thinking ‘so is it all in my mind?’
‘They said it was “all in my head”’
It is common for people with pain to feel they have been told that pain is imagined, psychological or all in their head. This in itself can be very upsetting. We asked a GP why people might leave the consultation room feeling this way:
‘GPs ask patients about how they’re feeling or how life is because we recognise pain can be affected by these factors, not that they’re the main cause. The skill we have to develop is reassuring them that we’re looking at all of the factors behind their pain, and it’s not that we think they’re mad.’
You might leave your consultation wondering:
- Why do they want to talk about how I am feeling?
- Why are they asking me about my life?
• Why won’t they focus on my pain?
Thinking about the bio-psycho-social model of pain helps to explain this – healthcare professionals ask these questions to get as full a picture as possible. Another GP said:
‘Knowing where they are in life, what their family situation is, other things that are going on in the family, what they might be worried about, how they feel they have to limit themselves or push themselves. You need to have that discussion with them.’
It does not mean the GP is not interested in the physical aspects of your condition. Looking at the full picture of your pain and how it affects you (including your emotional wellbeing) could mean that they are better able to help you manage the whole experience, putting together the different parts of the jigsaw.
How might chronic pain make me feel?
There is no ‘one-size-fits-all’ answer. Emotions and thoughts differ from one person to the next and over time. What we do know is that the emotional impact can be long lasting and overwhelming, partly because of changes to the brain caused by chronic pain. We spoke to a wide range of people with pain about some of the negative feelings and thoughts that they have experienced:
So I get the idea pain can affect my mood – so what?
People in pain often talk about ‘carrying on regardless’ or ‘pushing through’ and may feel that ignoring difficult emotions is the best approach. However, recognising some of the negative feelings and thoughts you may experience can be helpful in managing your pain in the long term, as well as reducing some of the suffering it can cause.
Managing your emotions
The close links between the centres of pain and emotion in the brain make it almost impossible to have pain without having negative emotions as well. Recognising the emotional impact of chronic pain can be a first step towards being able to manage both pain and emotions better. This might include becoming more aware of how you are feeling in the first instance. Becoming gradually more active, eating well, developing some better sleep routine strategies and planning for flare-ups can all help manage the emotional side of the pain.
People have found these things helpful in managing their emotions:
- DON’T STOP DOING THINGS. ACTIVITY CAN PROVIDE PLEASURE AND A SENSE OF ACHIEVEMENT, EVEN WITH PAIN
When you are feeling low you might not feel motivated to do the things that you usually enjoy, like spending time with family and friends and other social activities. However, avoiding enjoyable things can further entrench negative feelings. Try to keep doing the things you enjoy and spending time with the people you care about however discouraged you feel.
- TAKE A STEP BACK
When we feel low, we can often get caught up in believing a range of very negative things about our situation, the future or ourselves. Taking a step back to observe what you’re feeling and what you’re saying to yourself can often be helpful. We can see things more clearly from a distance sometimes.
- GIVE YOURSELF CREDIT FOR THE THINGS YOU HAVE DONE
Day-to-day activities and responsibilities become hard to fulfil when living with pain. It’s important to recognise what you ARE doing. No one can do everything every day.
Acknowledge whatever you’ve managed to achieve despite the pain. On your worst days try to find even very small things in the day that will give you a little bit of pleasure, or give you a small sense of achievement.
Instead of keeping a pain diary, what about making time each day to write in a journal for ‘My Achievements’. Make sure you give yourself the credit you deserve.
- IDENTIFY TRIGGERS AND LEARN TO MANAGE THEM
Very often the same patterns make us come unstuck. Look at what led up to the way you are feeling. Is there something (not necessarily the pain itself) that always triggers stress, upset, etc.?
How you react to things and what you say to yourself can trigger upset in the same way as the pain can. Is there a way to become more aware of the triggers so you can make a choice about how to respond?
- WATCH OUT FOR HOW THOUGHTS AFFECT YOUR STATE OF MIND. BE KIND TO YOURSELF!
Be aware of any tendency to judge yourself or your situation, or to assume that things will turn out for the worse or that others think badly of you. When in pain you may have a tendency to criticise yourself.
Simply becoming more aware of what you are saying to yourself can be helpful. It allows you to step back and see thoughts for what they are – just thoughts.
Could you learn to give yourself the support you would give to a close friend? Recognise and celebrate even small successes, gently encouraging yourself when the going gets tough.
- IT’S OK TO ASK FOR HELP AND ACCEPT IT WHEN IT’S OFFERED
To manage the intensity of pain we need a team of people around us who we can call on for support – family, friends, colleagues or neighbours. Who could you turn to on a really bad day?
If your mood is very low or you feel very anxious or frustrated, don’t expect to manage all of this and your pain by yourself. Speak to your GP or try a support group for people in pain in your local area.
Improving your mood is not a cure for chronic pain. Managing thoughts and feelings can be difficult and you may have to work on it for a while before you see any benefits. However, eventually, feeling more positive may reduce the pain and the amount of suffering associated with it.
David Craig
Dr Craig is a Consultant Psychologist at NHS Greater Glasgow and Clyde. He has over 20 years’ experience working in chronic pain services and leads NHS Greater Glasgow and Clyde’s community Pain Education Sessions.
Katy Gordon
During her time as Pain Concern’s research officer, Dr Gordon developed the award-winning Self-Management Navigator Tool. She is author of ‘Barriers to Self-Management of Chronic Pain in Primary Care’ (British Journal of General Practice, 2017) and contributed to ‘Communication and Relationship Building with People in Pain’ (Core Standards for Pain Management Services, 2021).



